Launceston Obstetrics & Gynaecology is able to offer the complete range of obstetric and gynaecological ultrasounds including 3D ultrasound.
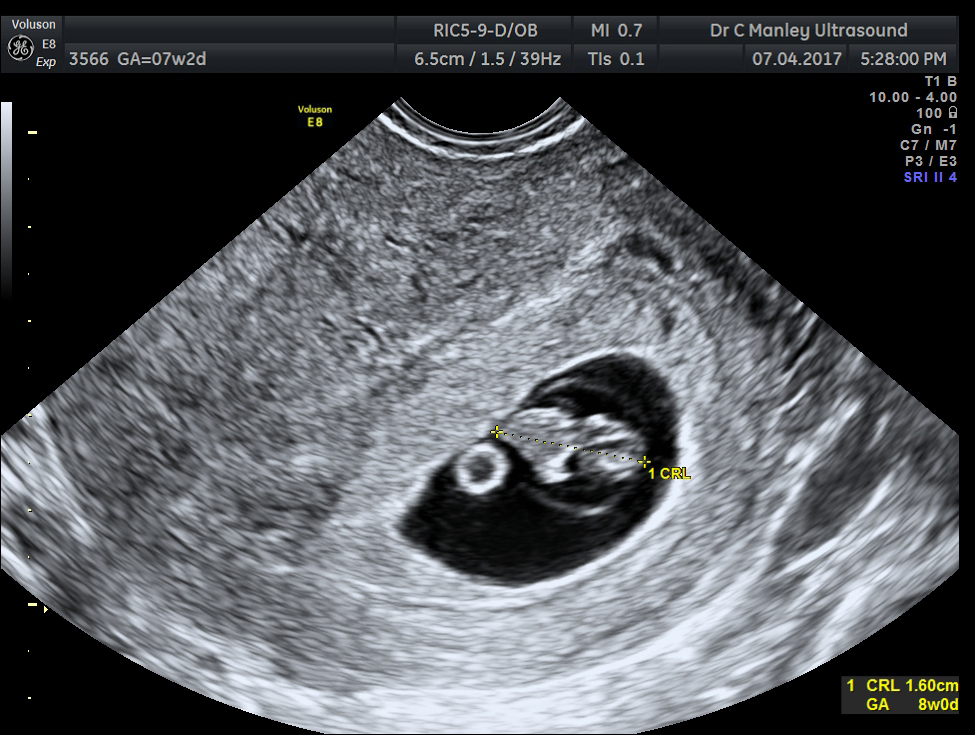
Dating scan
An ultrasound is performed generally from 7-11 weeks to confirm the due date, the number of embryos and to visualise the embryo’s heart beat and to confirm that the pregnancy is in the uterus. This scan may need to be done transvaginally depending on the position of the uterus and the stage of the pregnancy.
At 7 weeks’ gestation, a pregnancy sac should be seen within the uterus. Within the gestation sac, a yolk sac and an embryo with a visible heart beat should be present.
Sometimes it may be too early to gather the necessary information and a follow up ultrasound may be advised in 7-10 days.

The First Trimester Ultrasound
The 11-14 weeks’ scan provides important information about a pregnancy:
- The anatomy of the foetus can be assessed in great detail. Where previously patients had to wait until 20 weeks to find out if there was a major problem like spina bifida, anencephaly, a major heart defect or a similar serious condition, ultrasound technology has advanced so that such abnormalities can be identified much earlier. A transvaginal scan may be required for optimal views and is preferably performed between 12 weeks and 4 days and 13 weeks and 3 days.
- The nuchal translucency (NT) of the foetus is identified and measured during this narrow window of time. The NT is a collection of fluid between the skin and the soft tissues of the neck. It is often increased with Down syndrome and other chromosomal or congenital anomalies.
The First trimester combined screening test combines the age of the mother, the results of the ultrasound and the results of a hormone and placental protein in the mother’s blood (PAPP-A and beta hCG) to determine the risk of having a baby with Down syndrome and other chromosomal anomalies. The accuracy of detecting Down syndrome using this test is approximately 90%- 95%.
It is important to understand that a low risk screening result does not rule out an abnormality. Similarly, an increased risk result does not indicate that an abnormality is present. Instead, an increased risk result allows you the option to pursue further tests which may include chorionic villus sampling (CVS) or amniocentesis to provide a definitive result. - Pre-eclampsia risk assessment.
Uterine artery blood flow can be measured and combined with other maternal factors for pre-eclampsia risk assessment. Pre-eclampsia is a disease affecting the health of both mother and baby and is a cause of premature delivery. Preventative measures can be taken for those who screen at “high risk “.
Launceston Obstetrics & Gynaecology is an accredited ultrasound practice with RANZCOG to perform the 11-14 scan and perform the First Trimester risk assessment with annual auditing of results and sonographers.


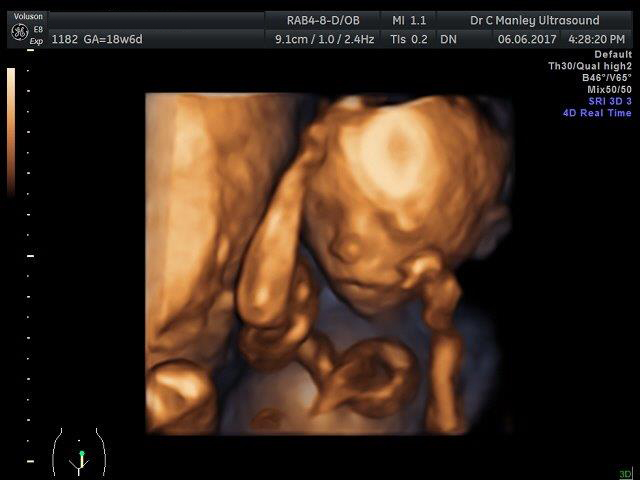
The Mid Trimester Ultrasound or Morphology scan
In Australia, a routine ultrasound examination is offered to most pregnant patients at 18-20 weeks. The purpose of this examination is to assess the:
- Foetal anatomy. This involves a detailed examination of the foetal brain, face, spine, heart, abdomen, renal tract, arms, legs, hands and feet and gender.
- Position of the placenta
- Amniotic fluid volume
- Pelvic anatomy and length of the cervix
This examination is expected to detect the majority of major foetal anomalies. It is important to appreciate that an ultrasound does not detect all abnormalities. Some abnormalities are progressive and unable to be detected at the 20-week ultrasound. Cerebral palsy, biochemical abnormalities and some chromosomal abnormalities cannot be detected.
Detection of abnormalities allows the options of further investigation, early postnatal treatment and delivery of high risk babies in tertiary centres, e.g. babies with congenital cardiac anomalies are further assessed by foetal echocardiologists in Melbourne to discuss likely outcomes, and delivery is usually planned in Melbourne where the newborn can receive neonatal cardiological treatment.
The views of the foetus may be limited by the:
- Foetal position at the time of the examination. Every attempt is made to visualise the baby but occasionally the patient will need to attend on another occasion to complete the study.
- Tissue interposed between the ultrasound probe and the baby (fatty tissue or fibroids) which absorbs the ultrasound waves. If diagnostic images are not obtained, the patient may need to be rebooked at a later date to further assess the foetus.
Please inform the sonographer at the beginning of the ultrasound if you do not wish to know the gender the foetus.


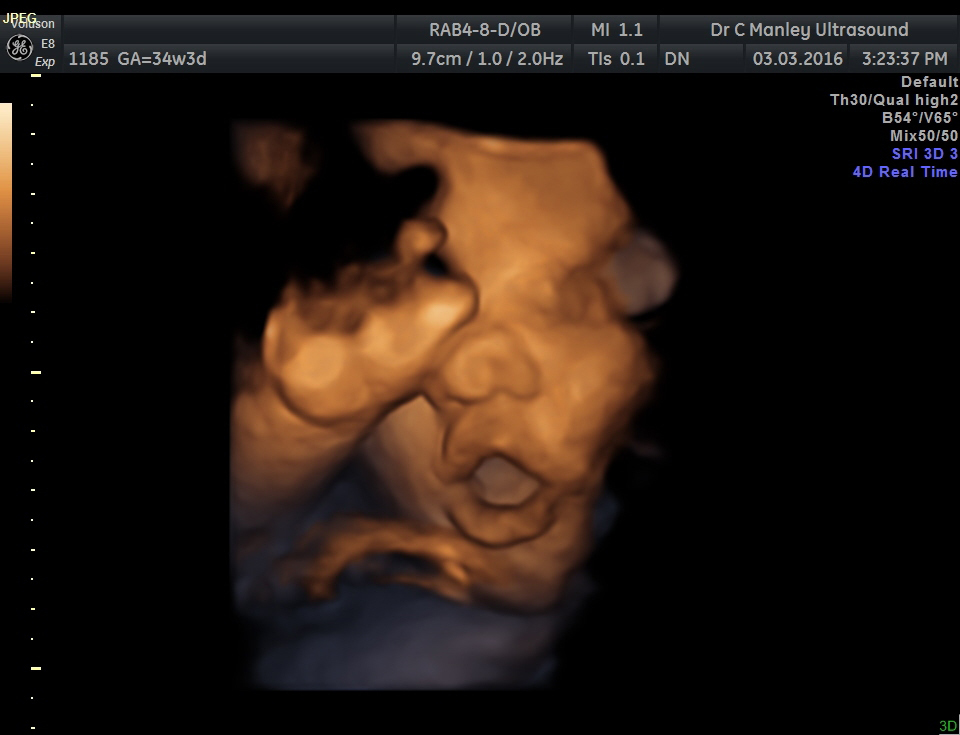
Third Trimester ultrasound or Growth scan
Some patients require a 3rd trimester ultrasound to:
- Check foetal growth
- Assess placental position
- Review findings from a prior ultrasound
An estimated foetal weight can be obtained from the ultrasound measurements, but variation can be +/- 400g.
If the foetus is optimally positioned, with a pocket of amniotic fluid in front of its face, true life 3D/4D images can be obtained. This may be limited if the foetus is larger, with a relative decrease of amniotic fluid.
3D and 4D Imaging
3D ultrasound produces a still, three- dimensional image of your baby, like a photograph within the womb. With 4D ultrasounds, the 3D image of the baby is seen to move. 4D gives a short video clip of your baby’s activity. Both 3D and 4D imaging are used for diagnostic purposes. Diagnosis takes priority in all our foetal assessments; however our specialist Obstetric Sonographers endeavour to provide patients with true to life pictures of their baby.


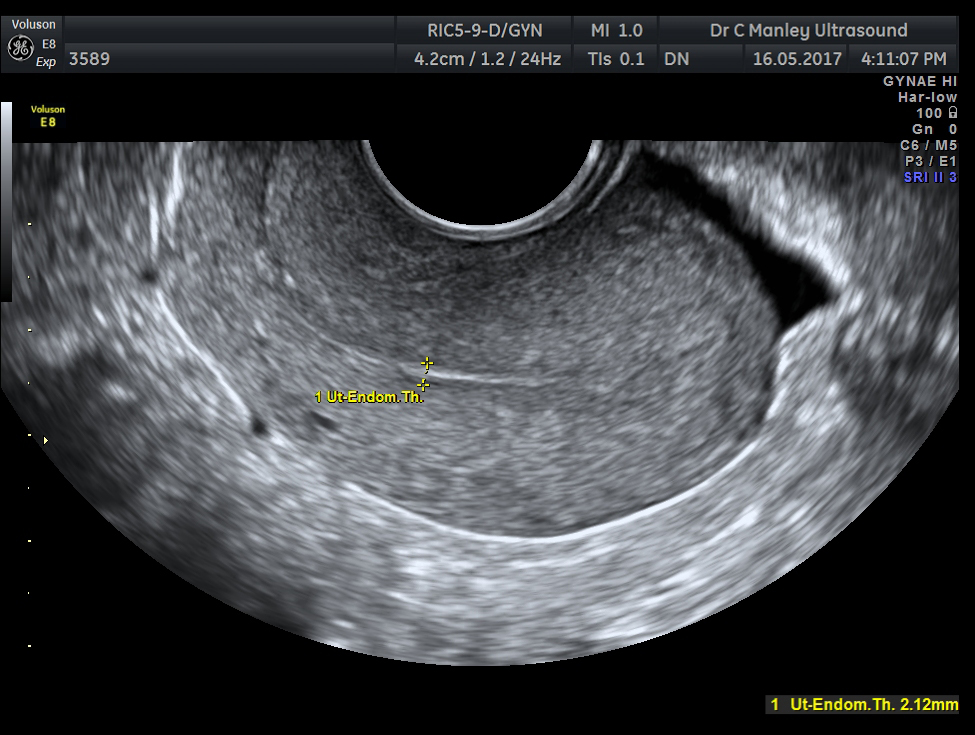
Pelvic or Gynaecological ultrasound
A pelvic ultrasound assesses the female reproductive system, including the uterus, ovaries, fallopian tubes, vagina, cervix and other pelvic structures. It can provide helpful information for those experiencing:
- Heavy, irregular or infrequent periods in the premenopausal woman
- Postmenopausal bleeding
- Infertility
- Assessment of pelvic masses like fibroids and ovarian cysts
A pelvic examination is initially performed transabdominally with a full bladder and then transvaginally after the bladder has been emptied.
Transvaginal ultrasound is performed using a special transducer which is slightly thicker than a tampon. It is covered with a disposable latex sheath and lubricating gel, then gently placed in the vagina and advanced under ultrasound guidance.
The probe sits in the vagina throughout the examination which usually takes 10-15 minutes. Most patients find the procedure much more comfortable than having a PAP smear.
During the examination, the specialist gynaecological sonographer may need to press gently on the abdomen to move bowel out of the way and bring the ovaries and other pelvic structures into view. This also enables any point of tenderness to be identified.
It is our protocol to offer transvaginal assessment for all gynaecological and most of early pregnancy scans. This is because the transducer is positioned close to the pelvic structures, producing superior images, and hence the most accurate diagnosis.
While it is our protocol to offer a vaginal scan, patients may decline and instead be scanned entirely transabdominally. In some circumstances a transvaginal ultrasound examination is not possible or advisable e.g. If a patient has not had sexual intercourse before, or if there is vaginal scarring or tenderness. Please discuss this with our specialist gynaecological sonographer if you have any concerns.